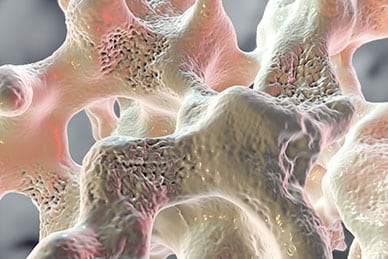
Osteoporosis is a disease where the density of your bones falls to a critical point where they are so weak that even mild physical impact can fracture them. Some people do not experience any symptoms of osteoporosis until they break a bone in a situation that would not have harmed them when they were younger. Osteoporosis is considered an age-related disease; osteoporosis is most common in women over the age of 50 and men over the age of 60.
Osteoporosis: Not Just a “Woman’s Disease”
It’s a fact that osteoporosis is much more common in women. This is true for several biological reasons. The sudden drop in estrogen levels that women experience during menopause causes their bone mass to rapidly deplete. Women also have smaller bones than men to begin with, so when bone mineral density starts to drop with age, women’s bones reach that critical weakness point much more quickly.
Unfortunately, because osteoporosis is far more prevalent in women, it is often considered somewhat of a “woman’s disease,” leaving osteoporosis in men under-recognized and under-treated. Indeed, one to two million men in the United States alone have osteoporosis, with an additional eight to 13 million men suffering from low bone mass that could lead to osteoporosis in the future. Approximately 13 percent of American men over the age of 50 will suffer at least one osteoporosis-related fracture in their lifetime. Though this rate is not as high as that of women, men are twice as likely to die after an osteoporosis-related hip fracture than women are. Therefore, awareness of male osteoporosis is an important public health concern.
What Causes Osteoporosis in Men?
 Of course, aging is the primary cause of osteoporosis. However, there are many other medical and lifestyle risk factors that can make you more likely to suffer from osteoporosis as a man. There are also some medical problems and other factors that can actually be the cause of your osteoporosis, rather than aging. The most common causes and risk factors for this disease in men include:
Of course, aging is the primary cause of osteoporosis. However, there are many other medical and lifestyle risk factors that can make you more likely to suffer from osteoporosis as a man. There are also some medical problems and other factors that can actually be the cause of your osteoporosis, rather than aging. The most common causes and risk factors for this disease in men include:
- age-related testosterone deficiency
- androgen deprivation therapy
- corticosteroid use
- excessive alcohol use
- low body weight
- low calcium levels
- low vitamin D levels
- physical inactivity
- previous bone fractures
- small body frame
- spinal cord injury
- tobacco use
One of the strongest risk factors for osteoporosis is heredity. If your father had low bone mineral density or osteoporosis, you are four times as likely to also eventually develop it. If both your mother and your father had it, you are almost eight times as likely to develop it with age.
There are also several less-common risk factors and causes of osteoporosis in males:
- anti-epileptic drugs
- chronic kidney disease
- chronic liver disease
- Cushing syndrome
- eating disorders
- HIV
- hypercalciuria
- hyperparathyroidism
- malabsorption (e.g. that caused by celiac disease)
- mastocytosis
- multiple myeloma
- organ transplantation
- osteogenesis imperfecta
- rheumatoid arthritis
- Type 1 or 2 diabetes
Treatment and Prevention
Osteoporosis can be prevented by making efforts to preserve your bone mineral density as you get older. It is especially helpful to achieve optimum bone strength before the age of 30, if possible.
Proper calcium and vitamin D intake are crucial for healthy bones. Men older than 50 years of age should get at least 1,200 milligrams of calcium daily. As for vitamin D, men over the age of 50 should get at least 400 IU daily, and men over the age of 70 need 600 IU. However, experts recommend that for the purposes of preventing osteoporosis, you should consume at least 800 IU of vitamin D daily. Getting enough calcium and vitamin D has been proven to reduce the risk of fractures by 12 percent.
Other nutrients that can help reduce your risk of osteoporosis are magnesium and vitamin K. Arguably, it is a good idea to take a daily supplement that contains all of these nutrients. However, even if you take a supplement you should also eat a diet designed for bone health. Important foods to eat include fortified dairy, all manner of vegetables, egg yolk, nuts, seeds, whole grains, fatty fish and mushrooms. Getting plenty of fiber is also important, as research shows that dietary fiber can help increase calcium absorption. This is likely because fiber causes food to be digested more slowly, giving your body more time to absorb the calcium.
To improve bone strength, you must also adjust your lifestyle if necessary. Abstain from tobacco, limit alcohol to two drinks per day, and engage in weight-bearing exercises at least twice a week.
All men over the age of 70 should receive regular osteoporosis tests, just to make sure. If you have any of the risk factors or medical problems described earlier, routine testing should start at the age of 50.
They say that an ounce of prevention is worth a pound of cure. However, for men who have already been diagnosed with osteoporosis, medical intervention is in order. A class of medication known as bisphosphonates is the principal treatment; these can be administered orally or intravenously. Furthermore, any medical conditions that could be causing or contributing to a man’s low bone mass should be addressed. For example, a man who has developed osteoporosis due to sex hormone deficiency should investigate the possibility of testosterone therapy.


